The Death of "Wild to Mild", the Rise of "Informed Consent", and a Growing Measles Crisis
The CDC’s "Wild to Mild" Flu Vaccine Campaign Was Already Tame—So Why Was It Canceled?
The Sudden Cancellation of “Wild to Mild” and the Push for “Informed Consent”
Last week, at the peak of one of the worst influenza seasons in years, the CDC abruptly canceled its “Wild to Mild” campaign, which highlighted how the flu vaccine can reduce the severity of illness, even if you still get sick.
I thought it was a thoughtful, effective campaign, aimed at informing and resetting public expectations about flu vaccination—emphasizing that while the flu shot isn’t perfect, it lowers the risk of severe illness, hospitalization, and death.
So why, in a week when 50,000 people were hospitalized with flu—the highest level in 15 years—and 86 children have died this season, was it suddenly shut down?
At least one source reports that new federal health leadership wants vaccine messaging to focus on promoting “informed consent” instead.
What is Informed Consent?
Informed consent is a fundamental principle in medicine. It ensures that before making a medical decision—such as getting a vaccine—a person fully understands their choice, including the benefits, risks, and alternatives. It also means having the opportunity to ask questions and receive accurate, evidence-based answers before deciding.
With that definition, the idea of promoting “informed consent” in vaccine decision-making sounds like a positive step, right?
People should have clear, accurate information about the benefits of vaccines, including how they protect against disease and improve health. There should be transparency about both common and rare risks and, just as importantly, the real dangers of not vaccinating, including hospitalization and death. They should also be aware of unproven alternatives, which have no demonstrated safety or efficacy.
But true informed decision-making should go even further. A KFF poll found that 96% of adults have encountered at least one type of health-related misinformation, including false vaccine claims. Effective communication must not only provide accurate information but also help people recognize and unpack misleading claims, showing why they are false, deceptive, and often driven by motives unrelated to health.
If “informed consent” messaging truly helps people make informed, fact-based vaccine decisions, it would be a welcome shift—because the extraordinary benefits of vaccines far outweigh the risks.
So, What’s the Problem?
The Risk of Disinformed Decisions
Informed decision-making should be about understanding accurate, evidence-based risks and benefits. But in practice, this concept can be weaponized—and it often is.
For years, vaccine cynics have used “informed consent” to push the false idea that the medical establishment hides certain “risks”, even when those “risks” have been thoroughly studied and proven to be minimal or nonexistent.
Elevating fictional or wildly exaggerated risks to the same level as real but extremely rare risks (which should be communicated transparently) creates false equivalence. Instead of helping people make informed choices, it manufactures fear and distrust, leading to disinformed decisions—or outright refusal.
If new “informed consent” messaging introduces exaggerated or false risks, then it’s not informed at all—it’s “disinforming” the public.
Public Health Messaging: Emphasizing Benefits to Drive Informed Decisions
For over a century, public health campaigns have emphasized the benefits of key health behaviors, such as:
Quitting smoking
Getting mammograms and colon cancer screenings
Wearing seat belts and helmets
Eating healthier foods
Why? Because often people aren’t aware of these benefits, and accurate, proactive messaging helps them make better, more informed health decisions.
In today’s era of disinformation overload, the public is bombarded with narratives about risk—some real and many imagined. Yet, they are often far less informed about the overwhelming benefits of vaccines and other preventive measures.
Health Decisions Aren’t Just Personal—They Impact Communities
One of the biggest challenges in vaccine communication is bridging the gap between individual and collective benefits.
In clinical and personal healthcare settings, conversations about vaccination often center on individual risks and benefits, but these decisions don’t happen in isolation. A vaccinated community is a healthier, safer place for everyone, reducing disease spread and protecting the most vulnerable.
Many of my patients choose to get vaccinated not just for their own health, but for their families, friends, and at-risk neighbors. For them, vaccination isn’t just a personal choice—it’s an act of care for others. That sense of connection and responsibility is a benefit in itself, reinforcing the idea that protecting others also strengthens our own well-being.
We live in an individualistic society, but our health is inherently interconnected. If public health messaging is truly about informed decision-making, it must reflect this collective reality—because when we protect each other, we all thrive.
Final Thoughts
True informed consent is essential in vaccine decision-making. Effective vaccine communication is about partnership—helping people make informed decisions while respecting their autonomy. It must be accurate and evidence-based, presenting both risks and benefits in the proper context—not amplifying false narratives or exaggerating rare risks. And yes, it will naturally highlight the benefits of vaccines—because those far outweigh the risks.
But if “informed consent” is used as a cover to inflate false risks, fuel vaccine hesitancy, or erode trust, then it’s not informed at all—it’s disinformation masquerading as transparency, leading to “disinformed” decisions rather than truly informed ones.
With measles outbreaks spreading, influenza surging, and public health challenges mounting, now is not the time to create more confusion and doubt.
Now is the time for clarity and accuracy.
Measles Outbreak Update: The Numbers Keep Climbing
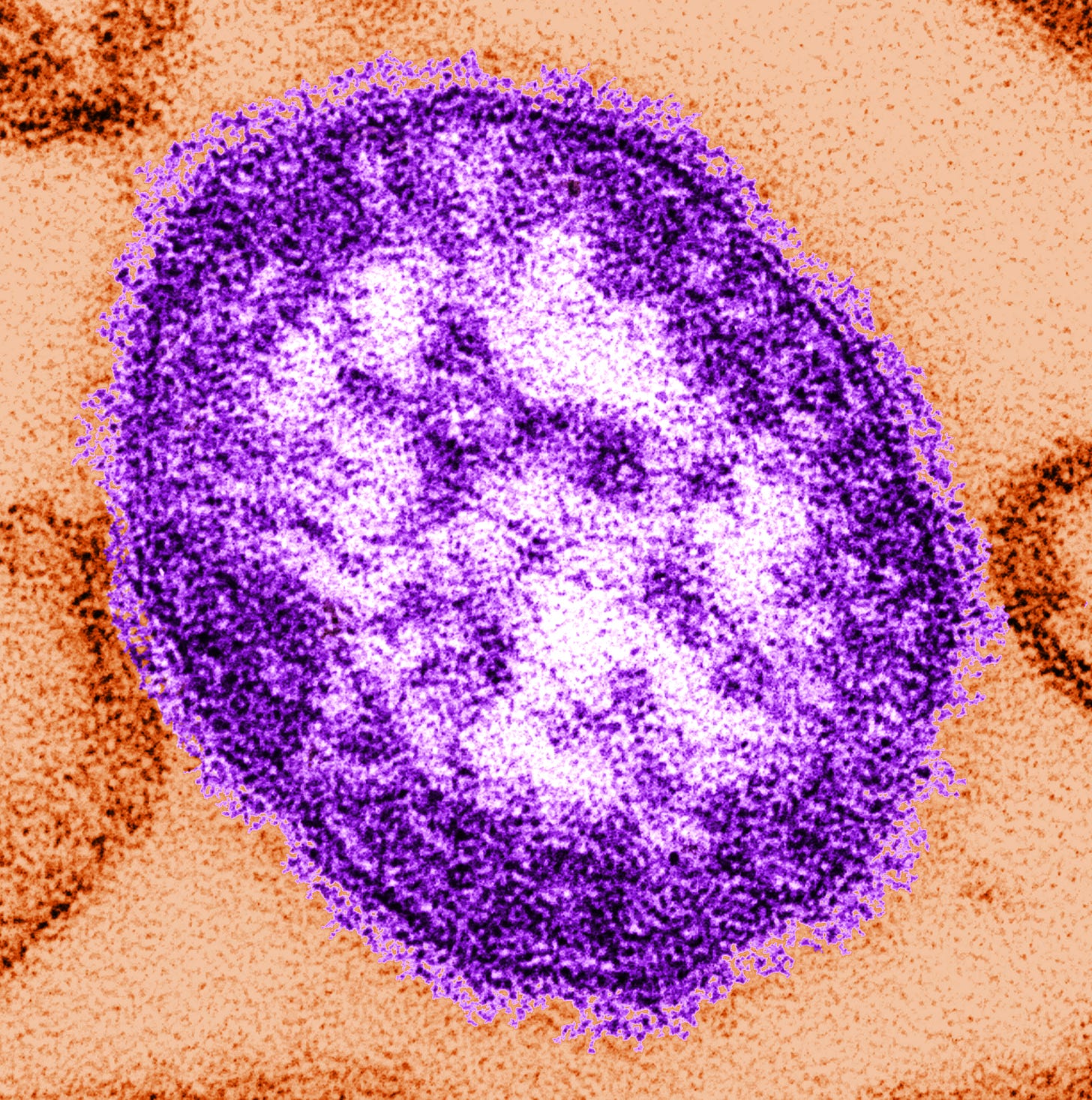
Last week I wrote about Texas experiencing its worst measles outbreak in over 30 years, with 58 confirmed cases and likely hundreds more undiagnosed. Now, the numbers have continued to rise, and the situation is even more concerning.
As of today, 100 cases have been confirmed, and the outbreak has spread beyond Texas. Measles—one of the most contagious viruses in the world—is spreading through under-vaccinated communities, endangering young children and other vulnerable individuals.
This should never happen in the U.S. Every illness, hospitalization, and dollar spent containing this outbreak was entirely preventable—with vaccines. When measles vaccination rates decline, it’s not a matter of if an outbreak will happen, but when. If we don’t take this moment seriously, it won’t be the last.
What I’m Watching This Week
• Will the “postponed” ACIP meeting actually be rescheduled?
• Will ACIP members be removed under the guise of past conflicts of interest, no matter how distant?
• Grant funding—including my own—is still stalled. Will there finally be movement in the review process?
• Will a preprint paper on COVID-19 vaccine “post-vaccination syndrome” continue to unecessarily spread fear?
• And most importantly—will spring ever arrive, or are we stuck in eternal winter?
YLE Webinar: Navigating Vaccine Conversations
If you missed it, last week I joined
and on a webinar to explore how to have meaningful, effective vaccine conversations— skills that are more important now than ever.This event (and recording) are a bonus for paid subscribers to YLE. I encourage you to check it out and become a paid subscriber to Your Local Epidemiologist!
Community Immunity is a newsletter dedicated to vaccines, policy, and public health, offering clear science and meaningful conversations for health professionals, science communicators, policymakers, and anyone who wants to stay informed. This newsletter is free for everyone, and I want it to be a conversation, not just a broadcast. I’d love to hear your feedback, questions, and topic suggestions—let me know what’s on your mind! And if you find this valuable, please help spread the word!