Hi community!
I’m so glad we had a nice, slow week in vaccine and public health policy—plenty of time to recharge and relax… Just kidding. It was another week for the record books!
Here are the highlights from this week:
Measles Outbreak Worsens in Texas & New Mexico: The measles outbreak continues to escalate, with nearly 200 cases in Texas and 30 in New Mexico, leading to multiple hospitalizations and two tragic deaths—one in an unvaccinated child and another in an adult. There is nothing “usual” about this outbreak—this is a preventable crisis.
RFK Jr.’s HHS Op-Ed Falls Short: Last weekend, the new HHS Secretary, RFK Jr., published an op-ed encouraging people to talk to their doctors about the measles vaccine and acknowledging its role in protecting individuals and communities. However, his message lacks what is most needed—an unequivocal, science-based recommendation to vaccinate!
CDC’s Plan to Study Vaccines and Autism: Despite decades of robust, peer-reviewed evidence debunking any link between vaccines and autism, the “CDC” (read between the lines) is reportedly planning a large-scale study on this already-settled question.
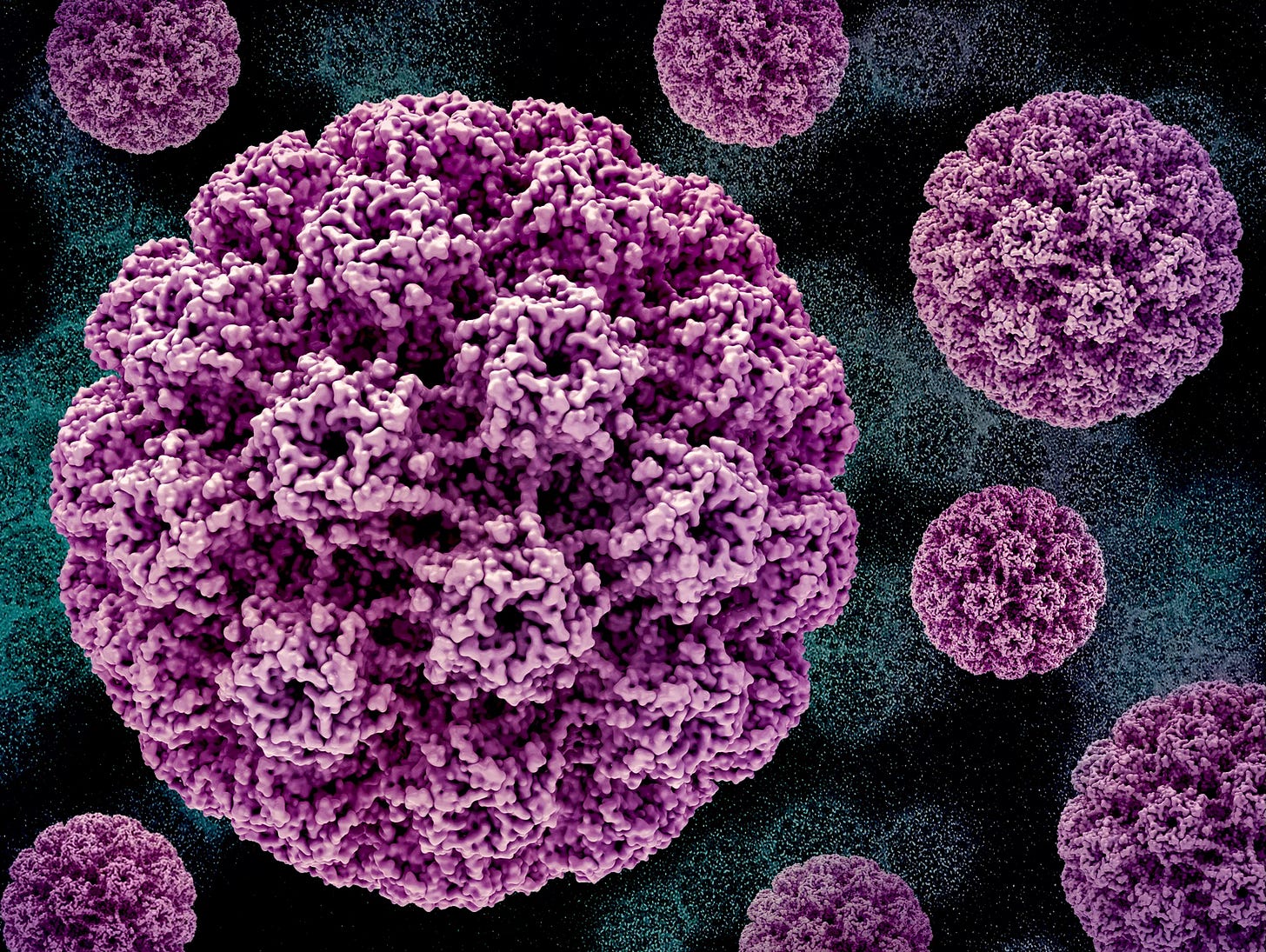
HPV Awareness Day: While measles is stealing the show this week, there are other important vaccine-preventable diseases! Last week (March 4) was HPV Awareness Day. I enjoyed teaming up with
and at to cut through the noise on the HPV vaccine with clear, evidence-based facts. Our article breaks down common concerns with solid scientific evidence and highlights the vaccine’s extraordinary real-world impact on preventing cancer.
Now here’s a closer look at these headlines, along with my insights and mostly unfiltered takeaways…
RFK Jr.’s Op-Ed: A Missed Opportunity
After widespread criticism from the scientific community—including myself—for downplaying the Texas and New Mexico measles outbreak as “nothing unusual” and highlighting vitamin A as a treatment (implying it as an alternative to vaccination), HHS Secretary RFK Jr. responded with an op-ed.
I appreciate that HHS now considers this a “top priority”, especially after it tragically claimed the lives of an unvaccinated child and an adult. However, if measles prevention is truly a “top priority”, then the Secretary must go beyond vague statements and recommending conversations—he must unequivocally endorse vaccination, the most effective way to prevent measles and protect families from unnecessary suffering.
Yes, he correctly acknowledged that the measles vaccine protects individuals and communities and encouraged people to talk to their doctors. But without a direct, confident recommendation to vaccinate, his message falls woefully short.
Am I surprised? Sadly, no.
What the Evidence Tells Us About Vaccine Communication
Decades of research show that one of the strongest drivers of vaccine uptake is a clear, confident recommendation from a trusted source such as a pediatrician or other health professional. The strength and quality of this recommendation is also important.
For some Americans RFK Jr. is a trusted source. If he truly wants to make this measles outbreak a “top priority”, he could do so in one simple step: unequivocally endorse vaccines.
Instead? His CDC is planning a large-scale study on vaccines and autism despite overwhelming evidence already proving no link—further fueling vaccine skepticism instead of stopping it.
Vaccines and Autism: A Needless Study That Fuels Misinformation
Apparently, dozens of large, rigorous, peer-reviewed studies confirming no link between vaccines and autism aren’t enough—because now, the “CDC” (or at least, the agency operating under its current leadership) is reportedly planning another large-scale study on this long-settled issue.
Here’s why this is a such a concern:
1. Do we really need another study? Absolutely not. We already have overwhelming evidence confirming no link—see for yourself: 25 studies here. At this rate, we may as well fund a massive trial to determine whether car seats prevent injuries in car accidents. Science has far more pressing questions that deserve funding. While funding for critical research, like childhood cancer studies, faces cuts, our federal health leaders are wasting resources reinvestigating long-settled questions instead of driving scientific progress forward.
2. Obvious confirmation bias: I have ZERO concern that a rigorous, peer-reviewed study will uncover something that dozens of previous studies haven’t. What DOES concern me is the very real possibility of a poorly conducted, biased, or politically influenced study that fuels more cynicism and misinformation rather than settling the issue.
Even the idea of this study reeks of confirmation bias—when researchers begin with a preconceived conclusion and selectively gather supporting data while dismissing contradictory evidence. I predict that they will find associations because by disregarding the overwhelming body of existing research, they are now actively searching for data to fit their narrative rather than letting the evidence lead the way. My only hope is that the career public health professionals and researchers tasked with this study stay true to the scientific process.
3. The mere act of conducting this study undermines public trust. It falsely suggests there is still scientific uncertainty when, in reality, this question has been asked and answered many times over.
4. Another wild prediction: If not published directly by the CDC, I predict this study will be published in The Journal of the Academy of Public Health—a publication with dubious editorial policies.
Skepticism vs. Science Denial
I fully expect people to push back at anyone who challenges the merits of this study, saying, “Science isn’t being open-minded!” But that couldn’t be further from the truth.
Dr.
recently wrote in The New York Times:“I’m an actual vaccine skeptic. In fact, everyone who serves with me on the FDA’s vaccine advisory committee is a vaccine skeptic.”
Healthy skepticism is a core part of the scientific process. My confidence in vaccines isn’t blind faith—it’s grounded in the rigorous research, exhaustive review, stringent approval processes, and ongoing monitoring that vaccines undergo. Each step is scrutinized, and skepticism is essential to that scrutiny.
When it comes to vaccines and autism, that scrutiny has already been applied, and the evidence is overwhelmingly clear. Re-examining this settled question—searching for a different answer—is not healthy skepticism; it’s cynicism and a waste of valuable research resources that could instead be used to address pressing health challenges.
An Example of Healthy Scientific Skepticism
Early in the pandemic, a reporter asked if I supported using COVID-19 vaccines for children while they were still in development. My answer seemed to catch them off guard—I told them I couldn’t say yet, though I hoped I would eventually be able to recommend them. They seemed to expect blind, unwavering support simply because I’m a pediatrician, the topic was vaccines, and I “believe in science.”
Unfortunately, this crucial part of the conversation is often overlooked. Rebuilding public trust in science requires transparency about the skepticism and scrutiny that are baked into the scientific process. Trust in science isn’t blind—it’s earned through a rigorous, transparent, and evidence-driven process.
Measles Outbreak Grows
The measles outbreak in West Texas and New Mexico is rapidly escalating, with nearly 200 cases in Texas and 30 in New Mexico—including dozens of hospitalizations and two deaths. These numbers are likely a significant undercount of the actual number of cases.
Measles is highly contagious but entirely preventable with the MMR vaccine, which has decades of safety and effectiveness data behind it. Yet, barriers to vaccine access, gaps in vaccine services, and rising hesitancy fueled by misinformation continue to drive outbreaks like this.
Our federal health leaders must take a clear, strong stance—vaccination is the most effective way to prevent measles and protect families from devastating complications and heartbreaking losses. There is no room for ambiguity when lives and community health are at stake.
HPV Awareness Day
Last week (March 4) was HPV Awareness Day, and I had the opportunity to team up with
and at to cut through the noise on the HPV vaccine with clear, evidence-based facts. Our article breaks down common concerns with solid scientific evidence and highlights the vaccine’s extraordinary real-world impact on preventing cancer. A few highlights:HPV vaccination prevents multiple cancer types, including cervical, anal, oropharyngeal, vulvar, vaginal, and penile cancers.
Real-world evidence shows a dramatic reduction in HPV infections (>85%), cervical precancers (80%), and early evidence of cancer prevention.
Recent studies demonstrate zero cases of cervical cancer among women vaccinated at ages 12-13.
The vaccine is recommended for both males and females, ideally at ages 9-12, before potential HPV exposure.
Check out our article and the other amazing science communication efforts
is doing here.Community Immunity is a newsletter dedicated to vaccines, policy, and public health, offering clear science and meaningful conversations for health professionals, science communicators, policymakers, and anyone who wants to stay informed. This newsletter is free for everyone, and I want it to be a conversation, not just a broadcast. I’d love to hear your feedback, questions, and topic suggestions—let me know what’s on your mind! And if you find this valuable, please help spread the word!