A Tumultuous Week: Measles, Vitamin A, Misinformation — And Rabies?!
Hi community,
It was another whirlwind of a week for vaccines and public health:
• The FDA’s VRBPAC meeting for next month was canceled.
• The first measles-related child death in over 20 years was reported.
• A flawed preprint article on COVID-19 vaccine side effects sparked controversy.
• Vitamin A as a measles treatment is trending.
• NIH legend Dr. Francis Collins retired.
• PubMed, ERA Commons, and other NIH websites went down over the weekend.
• The HHS Secretary took steps to reduce transparency.
Did I miss anything? Probably. I won’t cover everything, but I linked to insightful resources.
Vitamin A and Measles: A Dubious Messaging Misstep
Vitamin A supportive care for measles is suddenly trending, thanks to a recent CDC statement on the Texas measles outbreak highlighting its role alongside vaccination. The truth is, the World Health Organization recommends vitamin A for all children with measles, regardless of their country of residence, and many U.S. experts agree it should be given to all children with measles regardless of hospitalization status. And there is evidence that vitamin A deficiency worsens measles severity. (For more background, see this
post.)So, what’s the problem?
How this information is framed and communicated matters. Vitamin A is NEVER a substitute for the MMR vaccine, and we’ve seen similar messaging misused to fuel vaccine misinformation before.
• During a 2019 New York City measles outbreak, some community members relied on vitamin A (using spoonfuls of cod liver oil—gross) instead of vaccination.
• In a 2019 outbreak in Samoa, vitamins, including vitamin A, were wrongly promoted as a vaccine alternative.
As I told NBC News this week: “What I would have loved to see added in the CDC’s statement is that vitamin A is never an alternative to MMR vaccination for measles prevention. I think that clarity is really, really important.”
What didn’t make it into the article? This recommendation didn’t even need to be in a short general public statement. Since vitamin A is only used as supportive care after infection, who actually needs this information? A handful of physicians and families currently dealing with measles—not the general public. Amplifying it unnecessarily risks misinterpretation at best and fuels vaccine-alternative narratives at worst.
Measles Always Returns When We Let Our Guard Down
The first measles-related child death in over 20 years is a stark reminder that when vaccination rates drop, measles always returns—it’s not a matter of if, but when. And history shows that once the dangers become real again to people, vaccination rates do rise.
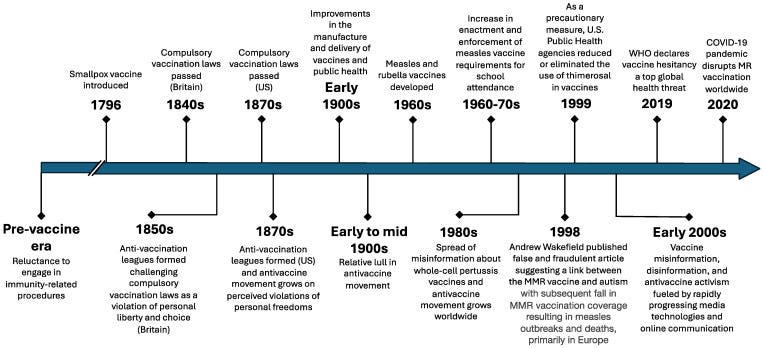
Vaccine hesitancy is not new. It is as old as vaccines themselves.
Image from Higgins DM, O'Leary ST. A World without Measles and Rubella: Addressing the Challenge of Vaccine Hesitancy. Vaccines (Basel). 2024 Jun 20;12(6):694. doi: 10.3390/vaccines12060694. PMID: 38932423; PMCID: PMC11209163.
Drops in measles vaccination due to hesitancy or access barriers have repeatedly led to surges in cases, followed by renewed immunization efforts. In the late 1970s and early 1980s, U.S. measles cases spiked until a national campaign restored high coverage. A similar pattern occurred in the UK and Ireland in the late 1990s and early 2000s after a falsified study linking the MMR vaccine to autism fueled vaccine hesitancy. More recently, in 2019, measles outbreaks surged worldwide, including in the U.S., prompting stronger public health interventions to boost vaccination.
But this cycle—drop, outbreak, rebound—is unacceptable. As I told The New York Times this week, “Every single outbreak, illness, hospitalization, and death is a tragedy, because it is entirely preventable with vaccines.” This should never be considered “usual”.
I shared several other thoughts on this earlier this week in an emergency post.
Rabies, Parent Panic, and the Perils of Vaccine Misinformation—Even for Pets!
Now for something completely different.
Recently, my daughter befriended a stray, uncollared cat that bit her. (No parent shaming, please!) As a pediatrician and preventive medicine physician trained in public health, I know the risks of rabies and the protocols for exposure. I should have calmly assessed the situation. Instead, as a dad, I freaked out—because, despite our training, doctors are just as human as everyone else.
Luckily, public health epidemiologists are incredible! Late on a Friday night (because, of course, these things always happen after hours), I called my local public health department. Within 15 minutes, the on-call epidemiologist called back. With expertise and empathy, they walked me through a plan, easing my fears in a way I desperately needed.
Public health workers rarely get the recognition they deserve. When they do their jobs well, no one notices. But that night, simply by doing their job, they were my hero.
Vaccines cause autism… in dogs?
This whole episode with my daughter made me think about this study last year which found that 37% of surveyed dog owners believe canine vaccines could cause autism—a claim with zero scientific basis. Unsurprisingly, those skeptical of human vaccines were also more likely to question pet vaccines.
The reality is that rabies is rare in the U.S. because of vaccines. Humans can get post-exposure vaccines, and we vaccinate pets to prevent its spread. Even wildlife get vaccines. Yet now, vaccine hesitancy is affecting pet owners too.
This puzzles me because it requires believing two completely false ideas:
1. Vaccines cause autism (thoroughly disproven).
2. Dogs can have autism (I'm not sure how this would even be studied as my veterinarian colleagues tell me that is not even a diagnosis in dogs).
This is a prime example of why better science communication is crucial. Misinformation isn’t just a human health issue—it’s spilling over into veterinary medicine, putting both pets and people at risk.
What I’m Watching This Week
Texas measles outbreak – Will community immunity slow it, or will we see more growth and, with it, tragic outcomes?
NIH website outages – PubMed and eRA Commons were down all weekend. A glitch, or something more? While they are back up this morning, this put a wrench in my academic writing plans this weekend!
Canceled ACIP and VRBPAC meetings – Will they be rescheduled, or will others step in to provide guidance? The critical issues they were planning to address, including the influenza vaccine composition for next season, cannot be “postponed” indefinitely. Although the FDA stated in a statement it would still weigh in on influenza vaccine composition, it did not clarify whether it would seek its advisers’ input or allow the usual public discussion and debate. While VRBPAC typically aligns with the WHO’s flu strain recommendations, this move further reduces transparency and erodes public trust.
NIH study sections were still cancelled last week – A colleague’s NIH study section was canceled last week, likely because it wasn’t announced in the Federal Register. While the hold has now been lifted, it came too late for the grants that were set for review. Hopefully, this won’t happen again.
HHS transparency rollback – The new HHS Secretary is reversing a rule that required public input on regulatory changes, contradicting his own transparency promises. Will this be challenged legally or politically?
Bird flu keeps spreading – Will it burn off? What’s the real pandemic risk? And can I still eat eggs—because I love them? I don’t know, but thankfully,
is keeping us informed here!Community Immunity is a newsletter dedicated to vaccines, policy, and public health, delivering clear science and meaningful conversations for health professionals, science communicators, policymakers, and anyone who wants to stay informed. We’ll navigate vaccine communication, misinformation, cynicism, and the policies shaping public health through evidence-based insights, real-world perspectives, and engaging discussions. This newsletter is free for everyone. If you find it valuable, subscribe below to support the effort and help spread the word!




I always appreciate your summary of what is happening in the realm of public health and vaccines! So glad you started a Substack - thank you!
Low beta carotene would go hand in hand with low vitamin C. Between 2016 and 2020 scurvy in children more than tripled from 8.2 to 26.7 cases per 100,000. Symptoms can include a rash that does not fade when you press a glass against it and sensitivity to light.